 |
年间契约型资讯服务
商品编码
1349830
头颈鳞状细胞癌 (HNSCC) - Tumor DeckHead and Neck Squamous Cell Carcinoma (HNSCC) - Tumour Deck |
||||||
头颈癌 (H&N) 的主要目标是起源于口腔的肿瘤,包括唇黏膜、咽、喉和鼻窦。 这些肿瘤95%以上是鳞状细胞癌。 口腔癌、下嚥癌、喉癌和非人类乳突病毒 (HPV) 相关口咽癌最常见的原因是吸烟和饮酒障碍。 头颈癌患者,尤其是烟草和酒精诱发的头颈癌患者,在头颈、肺部、食道、膀胱和其他接触这些致癌物质的部位同步发生原发性肿瘤,存在发生头颈癌的风险。第二原发肿瘤。
在先前的治疗(通常包括放射治疗和化疗)后疾病进展后,转移性头颈癌的治疗尤其具有挑战性。 过去四年,免疫疗法的批准和两种 PD-1 抑制剂用于治疗復发转移的批准令人兴奋。 临床试验目前正在进行中,并正在走向最终治疗。
头颈鳞状细胞癌不仅由癌细胞组成,而且是一个动态的生态系统,肿瘤细胞与微环境的各个组成部分相互作用。 这个生态系统包括免疫细胞、癌症相关成纤维细胞 (CAF)、癌症干细胞 (CSC)、脉管系统和病毒因子,例如人类乳突病毒 (HPV)。 了解这些成分之间的相互作用和串扰对于制定有效的治疗策略至关重要。
晚期肿瘤发生率相对较高,可能与HNSCC肿瘤早期患者症状有限或从早期向晚期进展较快有关。 高达 40% 的 cN0 颈部有隐性转移性疾病。 因此,开发用于早期检测转移的肿瘤生物标记至关重要。 肿瘤标记在二级预防中发挥重要作用。 可以使用生化和免疫学表达作为肿瘤标记来量化肿瘤分化。 目前,经过严格的体外测试,FDA 已批准 28 种生物标记用于临床。 然而,目前还没有 FDA 批准的 HNSCC 诊断或预后的蛋白质或突变标记物。
接受多种药物治疗的局部晚期 HNSCC 患者中,超过 50% 会在完成治癒性治疗后 3 年内復发或转移。 目前,由于没有有效的早期发现筛检方法,大量病例确诊时已属晚期。
本报告调查了全球头颈鳞状细胞癌 (HNSCC) 市场,并提供了市场现状、病例数趋势、患者趋势、竞争产品的市场定位以及市场机会。我是。
目录
第 1 章执行摘要
第 2 章头颈鳞状细胞癌 (HNSCC) 概述
- 头颈鳞状细胞癌 (HNSCC) 的定义、症状、病因和发病机制
- HNSCC 的分子变化
第3章头颈鳞状细胞癌(HNSCC)的定义与诊断
- 诊断生物标记
- 诊断演算法
第 4 章头颈鳞状细胞癌 (HNSCC) 流行病学
- 按国家/地区划分的盛行率
- HNSCC 国家阶段分类
第5章头颈鳞状细胞癌(HNSCC)的治疗实务
第 6 章核准的头颈鳞状细胞癌 (HNSCC) 标靶治疗
- 标靶治疗概述
- 头颈鳞状细胞癌 (HNSCC) 的未满足需求
- 疾病復发和/或转移率高
- HPV 阳性和 HPV 阴性 HNSCC 的治疗策略没有差异
- 目前标靶治疗面临的新挑战
第7章管道临床试验
- 头颈鳞状细胞癌(HNSCC)管状情形概述与分析
- 分子标靶治疗的临床进展
- 关键分子及临床试验结果
- 主要药物核准与上市的时间表
第8章三期资产
- 临床试验和结果
- 二期资产
- 临床试验和结果
第9章第一期资产
- 临床试验和结果
第 10 章头颈鳞状细胞癌 (HNSCC) 研发管线中的早期分子
第 11 章头颈鳞状细胞癌 (HNSCC) 研发管线中的非临床分子
第12章医生/KOL输入
- 来自美国、欧盟和日本 4 位 KOL 的见解
- 头颈鳞状细胞癌 (HNSCC) 的重大事件
- 扩大已核准的标靶治疗
- 订定新的可行目标
第 13 章头颈鳞状细胞癌 (HNSCC) 市场预测 - 2033 年
- 主要药物的市场预测与病患份额
第14章附录
Head and Neck (H&N) cancers primarily targets tumors originating from the oral cavity, including the mucosal lip, pharynx, larynx, and paranasal sinuses. More than 95% of these tumors are squamous cell carcinomas. The most common causes for oral cavity, hypopharynx, larynx, and Human Papillomavirus (HPV)-unrelated oropharynx cancers are tobacco and alcohol use disorders. Patients with H&N cancers, particularly those caused by tobacco and alcohol, risk synchronous primary tumors and developing second primary neoplasms in the H&N, lung, esophagus, bladder, and other sites exposed to these carcinogens.
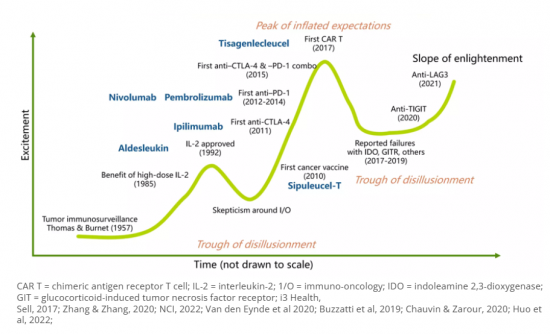
"Metastatic head and neck cancer is a challenging disease to treat particularly after disease progression on prior therapy, which usually includes radiation and chemotherapy. Over the last 4 years, we've seen the big excitement with immunotherapy being approved, with 2 PD-1 inhibitors approved in the recurrent metastatic setting. We're seeing this moving now to the definitive therapy setting with trials that are accruing."
Head and neck squamous cell carcinoma is not solely composed of cancer cells but is rather a dynamic ecosystem where tumor cells interact with various components in their microenvironment. This ecosystem includes immune cells, cancer-associated fibroblasts (CAFs), cancer stem cells (CSCs), vasculature, and viral factors such as human papillomavirus (HPV). Understanding the interactions and crosstalk between these components is essential for developing effective treatment strategies.
The relative higher incidence of advanced stage tumours could be related to limited symptomatology in patients with early stage or swift progression from early to advanced stage in HNSCC tumours. Up to 40% of cN0 necks harbor occult metastatic disease. Hence, developing tumour biomarkers to detect metastasis at early stage is essential. Tumour markers play a significant role in secondary prevention. Tumour differentiation can be quantified using biochemical and immunological representation as tumour markers. Currently, the FDA has approved 28 biomarkers after robust in vitro tests for clinical use. However, there is no protein or mutation marker approved for diagnosis or prognosis in HNSCC by the FDA
Mellalta Meets: Predictive Biomarkers of Checkpoint inhibitors
Predictive Biomarkers of Checkpoint inhibitors
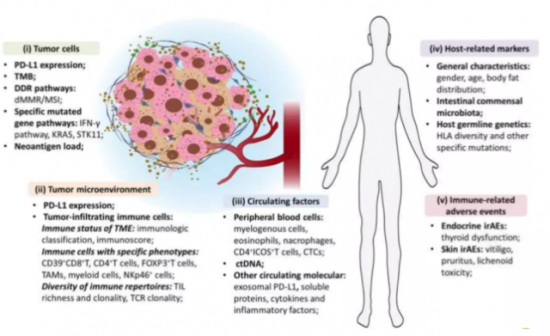
Source: Bai et al, 2020.
Mellalta's Head and neck squamous cell carcinoma (HNSCC) Deck: Current Treatment Landscape
The current standard of care for locally advanced (LA) HNSCC and recurrent/metastatic (R/M) HNSCC involves a combination of treatment modalities, including surgery, radiation therapy (RT), and chemotherapy.
For LA HNSCC, the primary treatment modality is often a combination of surgery and RT. In some cases, multimodal approach is considered in which chemotherapy may also be administered concurrently with RT to enhance its effectiveness.
For R/M HNSCC, the treatment options are more limited. Systemic therapy, which includes chemotherapy and targeted therapy, is the mainstay of treatment. Chemotherapy drugs such as cisplatin, carboplatin, and 5-fluorouracil are commonly used. Targeted therapies, such as cetuximab (an anti-EGFR monoclonal antibody), may also be used in combination with chemotherapy.
Immunotherapy has emerged as a promising treatment option for R/M HNSCC. Immune checkpoint inhibitors, such as pembrolizumab and nivolumab, have shown significant efficacy in improving overall survival in patients with R/M HNSCC.
Mellalta Meets Immunotherapies in HNSCC
"Management of early-stage locoregional HNSCC primarily rests on a combination of chemotherapy and radiation therapy. However, the therapeutic trajectory becomes intricate for patients experiencing local or regional recurrence due to radiation field overlaps. Additionally, the management of recurrent or second primary HNSCC has become more complex due to the increased incidence of HPV-associated HNSCC compared to non-HPV HNSCC. This change in disease profile has led to a wider range of treatment options available to practicing oncologists, further complicating the decision-making process."
Mellalta's Head and neck squamous cell carcinoma (HNSCC) Deck: Current Unmet Needs
- High rate of disease recurrence and/or metastasis and poor treatment outcomes severely affect long term survival: Over 50% of patients with locally advanced HNSCC who receive multimodal approached develop recurrent or metastatic disease within 3 years of the completing curative-intent treatments.
- Early detection of HNSCC is crucial for better treatment outcomes: Currently, there is a lack of effective screening methods for early detection, leading to a significant number of cases being diagnosed at advanced stages.
- No distinction in treatment strategy for HPV-positive and HPV-negative HNSCC which produces significant morbidity: HPV-positive and HPV-negative HNSCC distinctly differ genetically, they are treated in much the same way, an approach that produces significant morbidity. For patients with advanced-stage HPV-positive HNSCC, the 5-year survival rates are 75% to 80%, whereas fewer than 50% of patients with HPV-negative disease survive for 5 years.
- Diverse cases of Potential ICI resistance mechanisms in R/M HNSCC, which necessitates that many molecular targeted agents be tested in combination with ICIs
"Use of immunotherapy in the treatment of [HNSCC] is still evolving, with a continued unmet need for first-line regimens that provide durable clinical benefit with tolerable safety, further research is needed to determine the utility of dual immunotherapy as a treatment option for [HNSCC] and identify novel biomarkers to predict benefit with immunotherapy."
Mellalta's Head and neck squamous cell carcinoma (HNSCC) Deck: Key Takeaways
- Radiotherapy plus concomitant chemotherapy for fit patient's with unresected LA SCCHN (stage III-IV) has been shown to improve 5-year absolute survival by 6.5% compared with locoregional treatment alone.
- Despite of Cisplatin-Associated Toxicities, Cisplatin remains the radiosensitizer of choice for the majority of patients with locoregionally advanced head and neck cancer.
- Cetuximab is the only targeted therapy that has been proven effective for the treatment of HNSCC in both the LA and R/M settings. The incorporation of cetuximab not only expanded the range of treatment options in the past decade but also encouraged the investigation of many other targeted therapies in this tumor type.
- The current standard of care (SOC) in the second-line treatment of HNSCC typically results in an ORR of approximately 10-18%. There is room for improvement in the effectiveness of existing treatments.
Mellalta's Head and neck squamous cell carcinoma (HNSCC) Deck: Questions Answered:
- How can anti-PD-1/L1 therapies improve outcomes for patients with locally advanced HNSCC? Which combination strategies involving PD1-based therapies can drive change in recurrent/metastatic HNSCC?
- How can Merck Group's IAP antagonist xevinapant change the treatment paradigm for locally advanced HNSCC?
- How do oncologists view the role of Adlai Nortye's anti-PI3K agent buparlisib in the treatment of PD-1-refractory HNSCC?
- What are the key challenges and opportunities in the development of novel therapies for HNSCC, according to KOLs?
- Which companies are best placed to exploit the approach of novel IO-doublet regimens in HNSCC?
Table of Content
1. Executive Summary
- 1.1. Summary of future trends
- 1.2. Potential opportunities to explore.
- 1.3. Drivers/barriers for entry
- 1.4. What's new in HNSCC.
2. Head and neck squamous cell carcinoma (HNSCC) Overview
- 2.1. Head and neck squamous cell carcinoma (HNSCC) definition, symptoms, etiology, Pathogenesis
- 2.2. Molecular Alterations in HNSCC
3. Head and neck squamous cell carcinoma (HNSCC) Definition & Diagnosis
- 3.1. Diagnostic Biomarkers
- 3.2. Diagnostic Algorithm
4. Head and neck squamous cell carcinoma (HNSCC) Epidemiology
- 4.1. Incidence rates by countries
- 4.2. Stage specific cases of HNSCC by countries
5. Head and neck squamous cell carcinoma (HNSCC) Treatment Practices
- 5.1. Current treatment practices
- 5.2. Treatment algorithms
- 5.3. Summarized version of NCCN and ESMO treatment guidelines
- 5.4. Acceptable endpoints for accelerated approval?
6. Head and neck squamous cell carcinoma (HNSCC) Approved Targeted Treatments
- 6.1. Quick overview of targeted therapies
- 6.2. Unmet Needs in Head and neck squamous cell carcinoma (HNSCC)
- 6.3. High rate of disease recurrence and/or metastasis
- 6.4. No distinction in treatment strategy for HPV-positive and HPV-negative HNSCC
- 6.5. Challenges with the Current Emerging Targeted Therapy
- 6.6. To be Continued…
7. Pipeline clinical trials
- 7.1. Head and neck squamous cell carcinoma (HNSCC) pipeline landscape overview and analysis
- 7.2. Clinical Development of Molecular Targeted Therapy
- 7.3. Key molecules in clinical trials and results
- 7.4. Timeline of key drug approvals and launches.
8. Phase III Assets
- 8.1. Clinical trials and results
- 8.2. Phase II Assets
- 8.3. Clinical trials and results
9. Phase I Assets
- 9.1. Clinical trials and results
10. Head and neck squamous cell carcinoma (HNSCC) Pipeline Early-Stage Molecules
- 10.1. Phase I and Phase I/II molecules
- 10.2. Mechanism of action, trial dates, and topline results
11. Head and neck squamous cell carcinoma (HNSCC) Pipeline Non-clinical Molecules
- 11.1. Pre-clinical molecules
- 11.2. Mechanism of action, catalyst dates, and events
12. Physicians/KOLs Input
- 12.1. Insights from 4 KOLs in the US, EU, and Japan
- 12.2. Key Catalyst Events in Head and neck squamous cell carcinoma (HNSCC)
- 12.3. Expansion of approved targeted therapies
- 12.4. Creation of new actionable targets
13. Head and neck squamous cell carcinoma (HNSCC) Market Forecast -2033
- 13.1. Market Forecast and patient share by key drugs






